02.14.22
Two blood markers for schizophrenia
 |
This blog originated as a press release from the Swiss National Centre of Competence in Research SYNAPSY. Thanks to them for allowing us to repost it here. |
A research team from Synapsy has shown that the severity of the clinical symptoms of schizophrenia is strongly linked to blood biomarkers related to the deregulation of neuronal mitochondria.
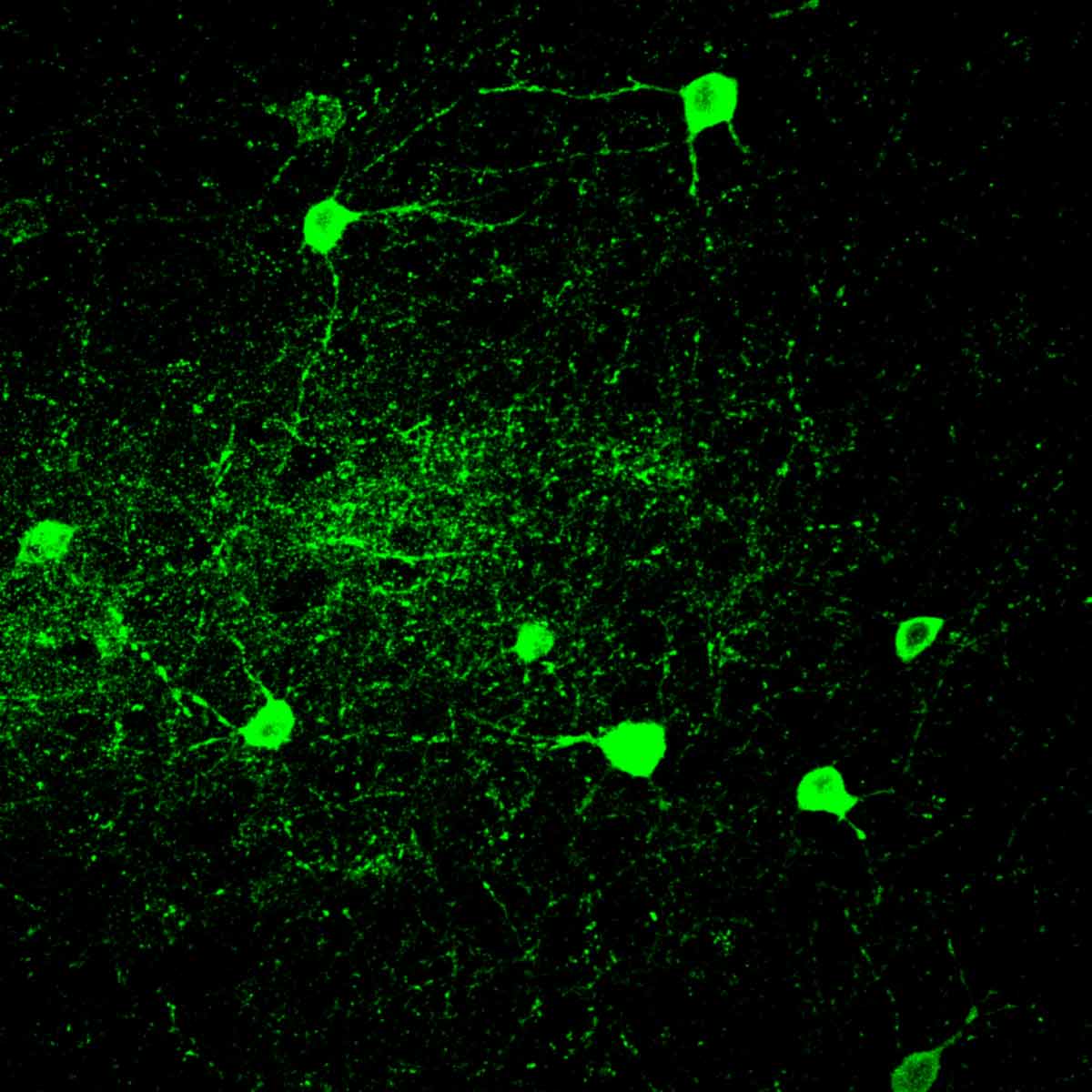
Psychotic symptoms are a characteristic clinical manifestation of schizophrenia. They go hand-in-hand with an increase in oxidative stress, which results in damage to a particular type of neurons called parvalbumin neurons. This deterioration leads to dysfunction in the activity of the prefrontal cortex, a region of the brain that is involved in cognition. A study conducted at the Centre for Psychiatric Neuroscience of the Lausanne University (UNIL) and the Lausanne University Hospital (CHUV), and supported by the National Centre of Competences in Research Synapsy (Synapsy), has shown, in an animal model, that the cellular mechanism for recycling mitochondria is deficient in parvalbumin neurons. The study – published in the journal Molecular Psychiatry – investigated the underlying biochemical mechanisms, pinpointing two key molecules, miR-137 and COX6A2, that can be detected in blood. When used as biomarkers in patients diagnosed with psychosis, they unveil two distinct clinical sub-groups with different severity of symptoms, cognitive deficits, and functioning in everyday life. This discovery represents a major breakthrough for stratifying individuals suffering from schizophrenia, whose heterogeneity of symptoms currently restricts diagnosis and treatment.