This post originally appeared in Bioquick News.
The 2018 annual meeting of the American Society for Exosomes and Microvesicles (ASEMV) was held October 20-24 in Baltimore, hard by the water’s edge in the Baltimore Marriott Waterfront Conference Center. ASEMV president, Stephen Gould, PhD, Professor of Biological Chemistry & Co-Director, Graduate Program in Biological Chemistry, Johns Hopkins, reported a record attendance of 250 scientists from the United States and around the world (Korea, Norway, Sweden, Canada, Australia, Japan, UK, Italy, Portugal, The Netherlands) at this historically intimate and highly interactive meeting that benefits greatly from having communal meals and no overlapping sessions. The five-day meeting featured over 100 podium presentations and myriad posters. The daily consecutive sessions typically ran from 8.30 in the morning to 9.30 in the evening, and were followed by two hours of poster viewing and interaction among researchers and with sponsors. The communal meals and poster sessions offered excellent opportunities for significant interaction amongst conference participants and also for interaction between attendees and the over 20 companies (see below) that were sponsors of the meeting. Dr. Gould highlighted the key role of these sponsors in enabling this very special meeting, and noted that this year featured record sponsorship, with almost triple the number of sponsors relative to the number for last year’s meeting at Asilomar in California. This impressive increase in sponsorship is a reflection of the recent explosion of research and interest in exosomes from many quarters of medicine and science.
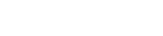
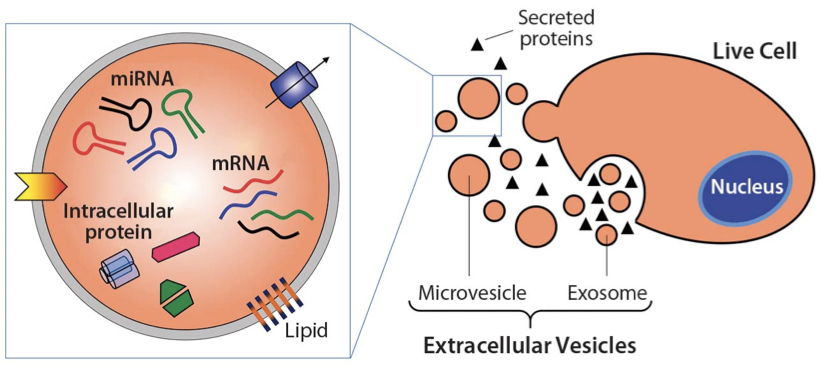
Among the themes of this year’s meeting was the growing appreciation for the heterogeneity of exosomes/microvesicles in terms of content, surface markers, size, and function. The similarities between exosomes and viruses were discussed in a number of talks. The brain’s use of exosomes for cell-to-cell communication within the brain, and also to communicate beyond the brain, was highlighted in multiple presentations. One of these suggested the dual promise of extracellular microRNAs in the diagnosis and pathology of Alzheimer’s disease. The role of exosomes in metastasis, carrying information from primary cancer cells to sites of future metastasis, was discussed and presented as further strong support for the century-old “Seed & Soil” hypothesis advanced originally by London surgeon Stephen Paget in 1889 (https://en.wikipedia.org/wiki/Stephen_Paget). Dr. Paget’s original article was titled “Distribution of Secondary Growths in Cancer of the Breast” (Paget, 1889).
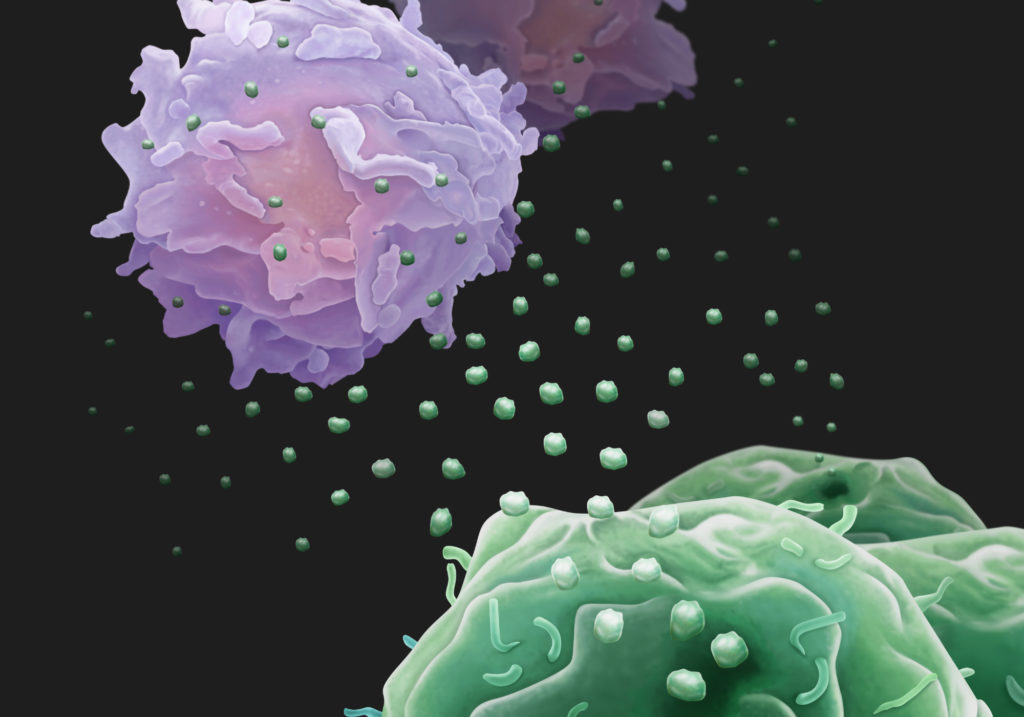
One presentation described EVs as epigenetic mediators of systemic communication in murine experimental sepsis and another, by sepsis expert Antonio De Maio, PhD, Professor and Member of the Biomedical Sciences Program at the University of California San Diego, described how phospholipids within EVs may contribute to the activation of target cells. Dr. De Maio, a graduate of the Central University of Venezuela in Caracas, had previously been Associate Professor and Research Director for the Division of Pediatric Surgery at Johns Hopkins, where he had also led the Committee for the Recruitment of Under-Represented Minorities to Graduate Programs. At UCSD, Dr. De Maio is also Director of the Initiative to Maximize Student Diversity Program at the university. At UCSD, Dr. De Maio’s laboratory focuses on the molecular and genetic bases of the response to injury.
Two presentations on tick exosomes and two on bacterial outer membrane vesicles highlighted the broad spectrum of exosome significance throughout the kingdoms of life. An opening night presentation suggested that vesicle-cloaked virus clusters are the optimal units for inter-organismal viral transmission.
The role of exosomes in glioblastoma was the subject of multiple presentations. Janusz Rak, MD, PhD, Senior Scientist in the Child Health and Development Program, and Professor, Department of Pediatrics, McGill University, began the Sunday morning sessions with a talk on the role of EVs in the evolution of glioma-initiating cells. Quantification of cancer EV populations using super-resolution microscopy was another highlight of Sunday morning talks.
ARC is repurposed retrotransposon Gag protein that mediates intercellular RNA transfer in brain
Paul Worley, MD, Professor of Neurology at Johns Hopkins and an expert on the molecular basis of learning and memory, with a focus on cellular mechanisms that support synapse-specific plasticity, opened the Sunday evening session with a highly stimulating discussion of how the neuronal gene ARC encodes a repurposed retrotransposon Gag protein that mediates intercellular RNA transfer. Dr. Worley described evidence suggesting that Gag retroelements have been repurposed during evolution to mediate intercellular communication in the nervous system. Previous work had shown that the neuronal gene ARC is essential for long-lasting information storage in the mammalian brain and mediates various forms of synaptic plasticity. ARC has been implicated in neurodevelopmental disorders. It has been shown that ARC self-assembles into virus-like capsids that encapsulate RNA. Endogenous ARC protein is released from neurons in EVs that mediate the transfer of ARC mRNA into new target cells, where it can undergo activity-dependent translation. Purified ARC capsids are endocytosed and are able to transfer ARC mRNA into the cytoplasm of neurons. ARC exhibits similar molecular properties to retroviral Gag proteins. Evolutionary analysis has indicated that ARC is derived from a vertebrate lineage of Ty3/gypsy retrotransposons, which are also ancestors to retroviruses.
Sensational Tuesday evening
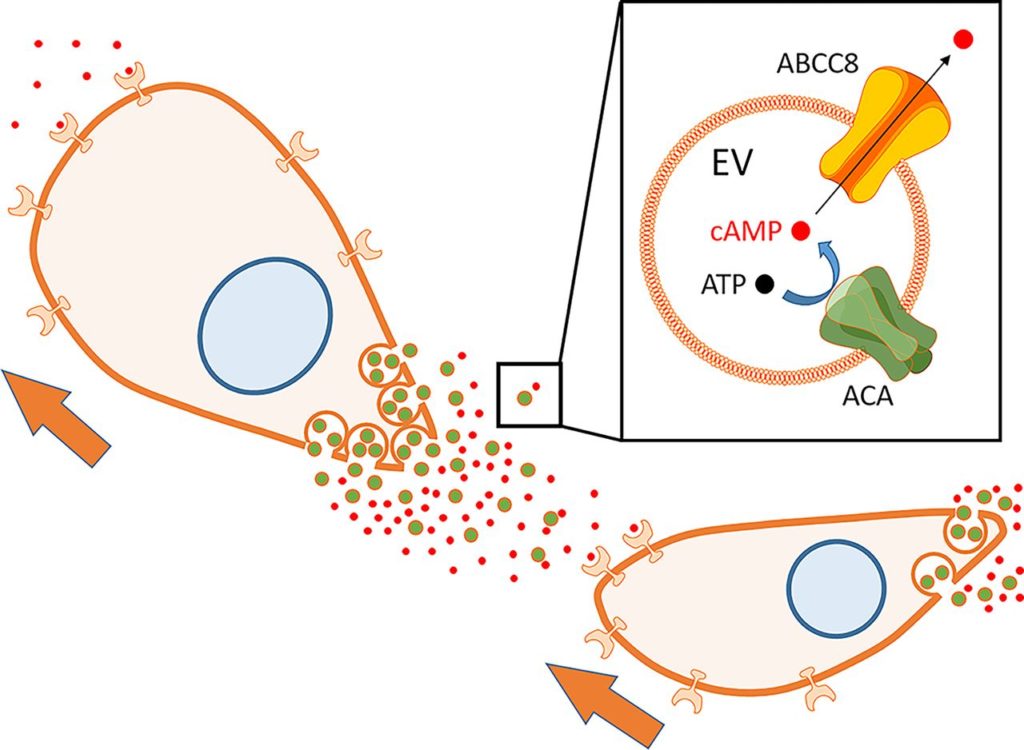
Tuesday evening featured a number of riveting presentations in a sensational session moderated by Xandra Breakefield, PhD, Professor of Neurology, Harvard Medical School, and Geneticist, Massachusetts General Hospital. A presentation on the use of machine learning-assisted histopathology to categorize large oncosomes held the audience spell-bound. Another suggested that EVs serve as delivery vehicles for LINE-1 retrotransposons.
Dr. Tushar Patel, Dean of Research at the Mayo Clinic-Jacksonville and an expert on liver cancer and liver transplants, had opened the session with a discussion of how biological nanoparticles might serve as therapeutic agents.
Other presentations in this session included ones on tools for live monitoring of exosome release from single cells, on the detection of mutant KRAS and TP53 DNA in circulating exosomes from healthy individuals and patients with pancreatic cancer, and on how an infected cell tolerates its viral pathogen using the exosomal pathway.
Beach Boys performance can’t distract ASEMV attendees
The attendees’ profound interest in exosomes was indicated on the opening evening of the meeting. At the outset, in outlining the logistics of the meeting, ASEMV president Dr. Gould explained that a late-breaking room change for Saturday night’s opening session had been occasioned by concern that the original room might be too noisy due to a performance taking place downstairs by The Beach Boys. The Beach Boys? Many thought that Dr. Gould was joking. But yes, the real Beach Boys were actually playing at a benefit event just downstairs from the ASEMV opening session, and yet, such was the audience’s interest in exosomes that no one moved. This reporter, however, could not resist checking out the iconic band after the opening ASEMV session had ended, and the photo here was taken of The Beach Boys who were indeed playing just downstairs. One of the original band members, Mike Love, was playing keyboard and singing. The Beach Boys performance was the highlight of a gala evening sponsored by Chimes (https://chimes.org/), a Baltimore-based international not-for-profit organization dedicated to assisting people with intellectual and behavioral challenges to achieve their fullest potential. It was an awesome backdrop to what would be an awesome ASEMV meeting.
Nearby International Human Virology meeting features major session on “Exosomes in health & disease”
And one further note is that the Institute for Human Virology (IHV), headed by legendary HIV virologist Dr. Robert Gallo, was holding its 20th International Meeting in the Four Seasons Hotel, right next to the Marriott where the ASEMV meeting was held.
Further indication of the exploding interest in exosomes was that the IHV meeting held a major session on exosomes this year. Titled “Exosomes in Health and Disease,” this session was listed second among nine sessions called out for special attention on the IHV meeting web page (https://www.ihv.org/ihvmeeting/). Areas of emphasis in this session ranged from cytokines in EVs to mechanisms of EVs in viral transmission.
Chairpersons of the IHV exosome session were Robert Gallo, MD, Director, Institute of Human Virology, University of Maryland School of Medicine, US, and Leonid Margolis, PhD, Senior Investigator, National Institute of Child Health and Human Development, US.
Speakers and topics included Xandra Breakefield, PhD, Professor of Neurology, Harvard Medical School / Genetist, Massachusetts General Hospital, “Extracellular Vesicle As Advance Forces in Cancer;” Dr. Margolis, “Not All Soluble Cytokines Are Soluble: Cytokines in Extracellular Vesicles Mediate Cell-Cell Communications;” Fatah Kashanchi, PhD, Former Director of Research, George Mason University, “Presence of HIV-1 RNA in Extracellular Vesicles from HIV-1 cART-Treated Cells;” Ayuko Hoshino, PhD, Instructor of Molecular Biology in Pediatrics, Weill Cornell Medical College, “Exosomal Protein Signatures: Mechanistic Insights and Biomarker Potential;” and Yoel Sadovsky, MD, Executive Director, Magee-Womens Research Institute, University of Pittsburgh, “Placental Exosomes in Maternal-Placental-Fetal Communication and Viral Resistance.”
Sponsors of ASEMV 2018 annual meeting
Sponsors of the ASEMV 2018 annual meeting included Particle Metrix, System Biosciences (SBI), iZON, Caris Life Sciences, nanoView Diagnostics, WAKO, ReNeuron, Norgen Biotek Corporation, Millipore Sigma, Beckman-Coulter, Wyatt Technology, AcouSort, Spectradyne, Fiber Cell Systems, ONI, abcam, Ceres Nano, Nanostics Precision Health, cellex, HansaBioMed Life Sciences, Lonza, and NanoTech.
Reference
Paget S. The distribution of secondary growths in cancer of the breast. The Lancet 133: 571-573. doi: 10.1016/S0140-6736(00)49915-0